Author: Dr Steve Nuttall | Posted On: 20 Aug 2024
Antimicrobial resistance (AMR) is a global health crisis, and Australia is not immune to its effects. As bacteria evolve to resist antibiotics, common infections become harder to treat, posing significant risks to public health. Recent data from the Australian Commission on Safety and Quality in Health Care’s AURA 2023 report sheds light on the current state of AMR and antibiotic prescribing in the Australian healthcare system.
Antibiotic Resistance Trends
The AURA 2023 report reveals concerning trends in antibiotic resistance among key pathogens.
Of particular concern is the rise in resistance to multiple antibiotics in Streptococcus pyogenes, a common cause of throat infections. The chart below illustrates this alarming trend:
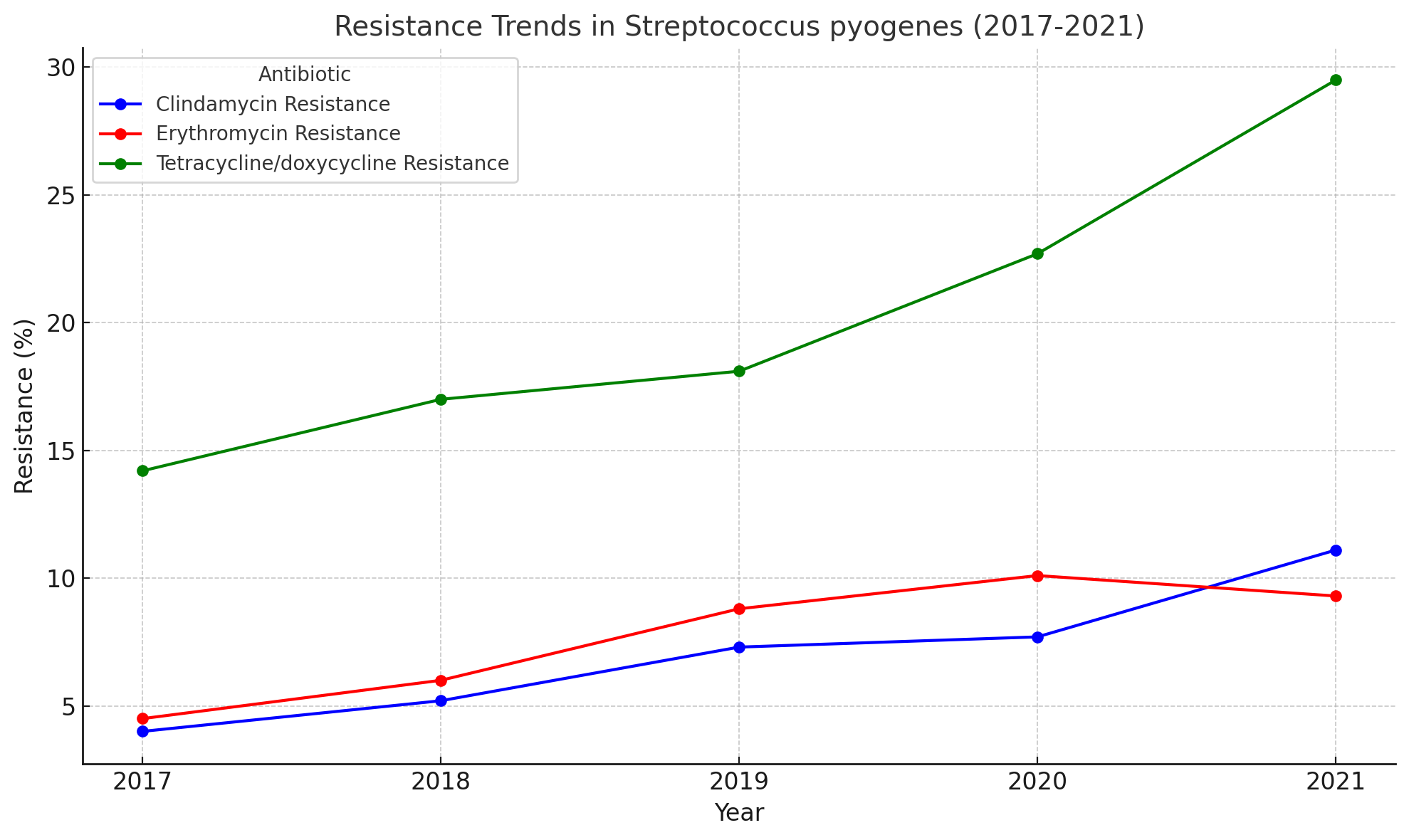
Most notably, tetracycline/doxycycline resistance has shown a dramatic increase, rising from 14.2% in 2017 to 29.5% in 2021. This steep upward trend is particularly concerning, as tetracyclines are often used as alternative treatments for patients allergic to penicillin or in cases where first-line treatments fail.
The graph also shows resistance to both clindamycin and erythromycin in S. pyogenes has increased significantly from 2017 to 2021. Clindamycin resistance more than doubled from 4.1% to 11.2%, while erythromycin resistance doubled from 4.5% to 9.3% (AURA 2023, Table S4.48).
The implications of this trend are concerning. S. pyogenes is responsible for a range of infections, from common strep throat to more serious conditions like scarlet fever and rheumatic fever. The rising resistance to these key antibiotics means that treating these infections is becoming increasingly challenging, potentially leading to longer illness durations, more complications, and the need for more potent, broad-spectrum antibiotics.
The sharp increase in tetracycline/doxycycline resistance is especially worrying as it limits treatment options for patients who cannot use other antibiotics. This trend may force clinicians to rely on newer, more expensive antibiotics, potentially increasing healthcare costs and the risk of developing resistance to these last-resort treatments.
Antibiotic Prescribing Rates
In the context of these trends in AMR, Australia’s high rate of antibiotic prescribing compared to other OECD countries is worrying. According to the latest OECD health care quality and outcomes indicators for Australia, the total volume of antibiotics prescribed for systemic use in 2022 was 27.6 defined daily doses (DDD) per 1,000 population per day. This is significantly higher than the OECD average of 15 DDDs per 1,000 population per day, with Australia having the highest rate among reporting OECD countries.
Whilst Australia’s antibiotic prescribing rate has decreased from its peak of 34 DDDs per 1,000 population per day in 2014 and 2015, it remains substantially higher than most other OECD nations. This high rate of antibiotic use is particularly worrying in the context of increasing antimicrobial resistance and underscores the urgent need for more judicious antibiotic prescribing practices in Australia.
Regulatory Changes and Pharmacist Prescribing
Australian pharmacists have recently gained the ability to prescribe antibiotics and other medications under specific conditions through various state-level pilot programs and regulatory changes. These developments are part of a broader initiative to enhance access to healthcare by utilising pharmacists to their full scope of practice.
While this change aims to improve healthcare accessibility, it also raises questions about its potential impact on antibiotic resistance. As pharmacists take on this new role, it will be crucial to ensure they receive adequate training in antimicrobial stewardship and follow strict guidelines for antibiotic prescribing.
Conclusion
The fight against antimicrobial resistance in Australia requires a multifaceted approach. The rising resistance rates in key pathogens, as dramatically illustrated by the S. pyogenes data, remain a significant concern. Continued surveillance, research, and public health initiatives are crucial to preserving the effectiveness of our antibiotic arsenal.
As we move forward, it’s essential to balance the need for accessible healthcare with the imperative to combat AMR. The expanded role of pharmacists in antibiotic prescribing presents both opportunities and challenges in this ongoing battle.
At Fifth Quadrant, our healthcare research capabilities offer valuable insights into how GPs and pharmacists are adapting to AMR concerns. We help pharmaceutical companies understand the changing patterns in recommending non-prescription products as alternatives or companions to antibiotics. Our capabilities include tracking trends in HCP recommendation of over and behind the counter brands, providing actionable intelligence for marketing strategies in this evolving healthcare landscape.
The Fifth Quadrant team is highly experienced in conducting healthcare market research. To learn more about our capabilities or if you have a brief to share, please get in touch
Posted in Uncategorized, Healthcare, QN

